Justin Sacks, MD, MBA, FACS

Justin Sacks, MD, MBA, FACS, is a plastic and reconstructive surgeon. His areas of specialty include reconstructive microsurgery following oncologic surgery, post-traumatic injury, as well as reconstructive surgery of the body, including the head and neck, breast, chest, abdomen, pelvis and extremities. He also has a passion for aesthetic surgery.
Dr. Sacks sees patients at:
Center for Advanced Medicine
Plastic and Reconstructive Surgery Center
4921 Parkview Place, Suite 6G
St. Louis, MO 63110
Barnes-Jewish West County Hospital, Medical Building 4
1044 North Mason Road
Creve Coeur, MO 63141
Please call 314-362-7388 for an in-person or video visit
What happened in the course of schooling to influence you to choose your specialty?
I grew up wanting to be a pediatrician. When I finally got to medical school, I realized that while I loved kids, but I didn’t necessarily want to take care of them as a doctor!
I quickly gravitated toward the idea of doing surgery and considered orthopedic surgery or general surgery. But a shift occurred the day I watched a gynecologist/ oncologist perform a specific cancer operation.
During the procedure, the plastic surgeons came into the operating room. At the time, I didn’t know what plastic surgeons were or why they were there. They literally moved tissue from one part of the patient’s body to the next, to help the reconstruction.
I saw something I had never seen before, and realized plastic surgery was an art and a science – requiring real creativity. I saw it as a specialty that allowed me to think about the whole human body – how it looks and how it functions. I immediately gravitated towards plastic and reconstructive surgery as a way to put people back together in both form and function — as well as being able to contribute as a researcher and teacher.
What brought you to Washington University?
I’m originally from New York City. I attended public school in New York, did my medical training in New York, Pittsburgh, and at MD Anderson Cancer in Houston. I had my first faculty position at MD Anderson and spent the last decade at Johns Hopkins in Baltimore.
What brought me here was the chance to lead a historic plastic surgery division at an incredible health care institution and medical school. The opportunity to become the Chief of Plastic and Reconstructive Surgery program that was run by Dr. Susan MacKinnon for the last 23 years, was something I could not pass up. I am excited to build upon that leadership of clinical expertise and scientific investigation.
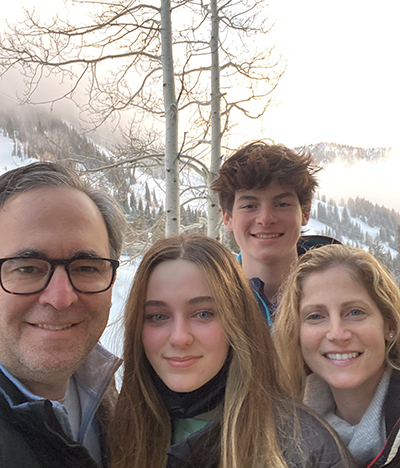
I arrived in St. Louis in February 2020, about one month before the pandemic shut everything down. My family arrived in June, and I can tell you, being without my wife (Dr. Bethany Sacks, who is a general surgeon here at WashU) and two children made that time the hardest five months of my life. Combine a pandemic, a new city and a new job – what an experience this has been.
This place is such a great institution and everyone is fantastic, it has been so much fun. I am honored and humbled to be in this position at this point in my life.
Which aspect of your practice is most interesting?
The aspect of my practice that is most interesting is that every day I wake up, get to come to work, take on different challenges and solve new problems that sometimes we have never seen before. Or I get to figure out ways to improve on something I’ve done before, in order to do it better. We put people back together after cancer and trauma has ravaged their body. There is nothing more noble I could do as a surgeon.
As a plastic surgeon, we operate head to toe and work with all the specialties from cancer reconstruction to traumatic reconstruction to cosmetic reconstruction – we are always trying to create something better with form and function.
What is the most challenging type of reconstructive surgery you perform?
Microvascular reconstructive surgery is the transfer of tissue– skin, fat, muscle, bone and nerves. This tissue is disconnected from arteries and veins in one part of the body and reconnected to other parts of the body.
The microsurgery involves sewing tiny blood vessels together using a microscope and sutures that are thinner than a human hair. To me, microvascular surgery is the most challenging because if the blood vessels don’t work, then the operation doesn’t necessarily go forward. Of all the surgeries I do, microsurgery can be all or nothing, and that makes it very challenging.
I constantly push myself to be at the top of my game and push my fellows, residents, and other faculty around me to be the best they can. It is so important we are able to deliver this high quality and sophisticated care for the cancer and trauma patient.
What new developments are you most excited about?
We’ve begun a lymphedema surgery program here at Washington University — this was something I started at Johns Hopkins. Lymphedema is caused by improper functioning of the lymph system that results in extreme swelling in arms and legs because they become filled with fluid and fat. Previously, the only treatment available to patients was therapy.
Lymphedema surgery is the rewiring the anatomy of the lymphatic system to help better drain and reduce the volume of fluid from the arms and legs. It is a very challenging microvascular surgery because these lymphatic vessels are smaller than a millimeter (a centimeter is the width of your little finger and a millimeter is 1/10th of a centimeter).
The surgery reduces the need for compressive garments and also reduces the potential for developing soft tissue infections like cellulitis. We have a very strong working collaboration with radiology, medicine, and occupational and physical therapy to help these patients.
Other new developments we are very excited about include state-of-the-art breast reconstruction using free tissue transfer with lymphedema surgery.
Limb preservation surgery is a new collaboration with vascular surgery, acute and critical care service and podiatry. For patients who might need an amputation, we work together to salvage the leg. Vascular surgery does the bypass, podiatry does the wound care and we do tissue reconstruction to optimize the length of the leg.
We are also working with researchers and tissue engineering specialists to explore ways to possibly eliminate some surgeries in the future – creating methods to modulate human tissue so that patients can help repair themselves.
Have you seen any impact on your practice with COVID?
When I first arrived here in February 2020, ahead of the pandemic, we were busy, especially with breast reconstruction after cancer surgery. Once the pandemic hit, some of our patients couldn’t benefit from the collaborative approach between breast oncology and plastic and reconstructive surgery for immediate reconstruction.
We have since rebounded and adapted to deliver optimal and coordinated care — and have increased the operating room schedule to seven days a week. We are working to get all our patients who need care back into the hospital.
Where are you from?
I was born in New York City and grew up in Brooklyn, New York. I’m a product of the New York City public school system.
For college, I headed upstate to Cornell University, went to medical school and did my residency in New York City at Mount Sinai School of Medicine. From there I’ve lived in Pittsburgh, Houston, Baltimore and now St. Louis, Missouri. I’ve had a lot of zip codes!
I am a native New Yorker living in the Midwest for my first time. What they say about the Midwest is 100% true — everybody is super nice and everybody works really hard. I love that!
Is there a particular award or achievement that is most gratifying to you?
I’ve been honored to receive many awards in my career through the hospitals I’ve worked and medical schools I’ve attended. I would say the most gratifying awards I’ve achieved have been my teaching awards I received when I was Vice Chief in the department of plastic surgery at Johns Hopkins.
I put a lot of energy and work into what I do, and that includes teaching and training medical students, residents and fellows how to be surgeons. To be recognized for that at the highest level is very gratifying and humbling.
What is the best advice you’ve received?
Dr. Lester Silver was my former chief when I was a plastic surgery resident at Mt. Sinai School of Medicine in New York City. He is no longer chief, but still works every day at the hospital! He’s still there first in the morning and probably last to leave at night.
He once told me, “You can’t dance at every wedding.” What that means is you can’t do everything — you have to pick the time and place you really want to be and put your best effort in. That was many years ago, but I always remember it and give that same advice to people when I’m mentoring them. If you say yes to everything, you are trying to do too much and sometimes that holds you back. That was the best advice I’ve ever received.
If you weren’t a doctor, what would you like to be doing?
As a kid, I was always passionate about architecture – building and designing things. So when I was younger, if I could not have become a doctor, I would have gravitated towards architecture.
But, if today you told me I couldn’t be a doctor, I would become a writer. I’ve kept notes on every single operation I’ve done – from the patient, to the diagnosis to the procedure. I would write about the experiences and the tens of thousands of lives I’ve touched and that have touched me. I’ve had the awesome privilege to be a part of my patients’ lives, and I have thousands of stories to write if I ever stop doing this.